Sexual health is often discussed in fragments. Some conversations focus only on performance, others on pregnancy prevention, and many avoid the subject altogether. Physicians say this piecemeal approach leaves large gaps in understanding, which in turn fuels anxiety, stigma, and preventable health risks. In clinics, doctors repeatedly hear the same assumptions: if nothing looks wrong, everything must be fine; if desire changes, something is broken; if contraception is in place, protection is complete. The reality is more nuanced, and far more human.
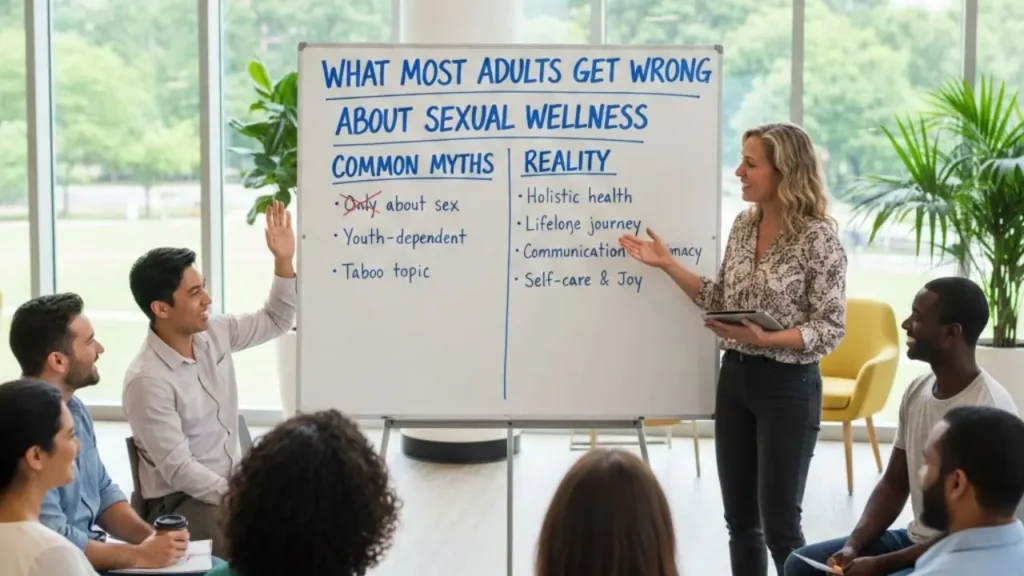
Sexual Wellness Myths Doctors Want Adults To Stop Believing
Medical professionals emphasize that sexual wellness involves the body, the mind, and the quality of communication between partners. Misunderstandings can prevent people from seeking testing, treatment, or simple reassurance. Clearing up these myths is not about judging behavior; it is about giving adults accurate information so they can make safer, more confident decisions and build healthier relationships.
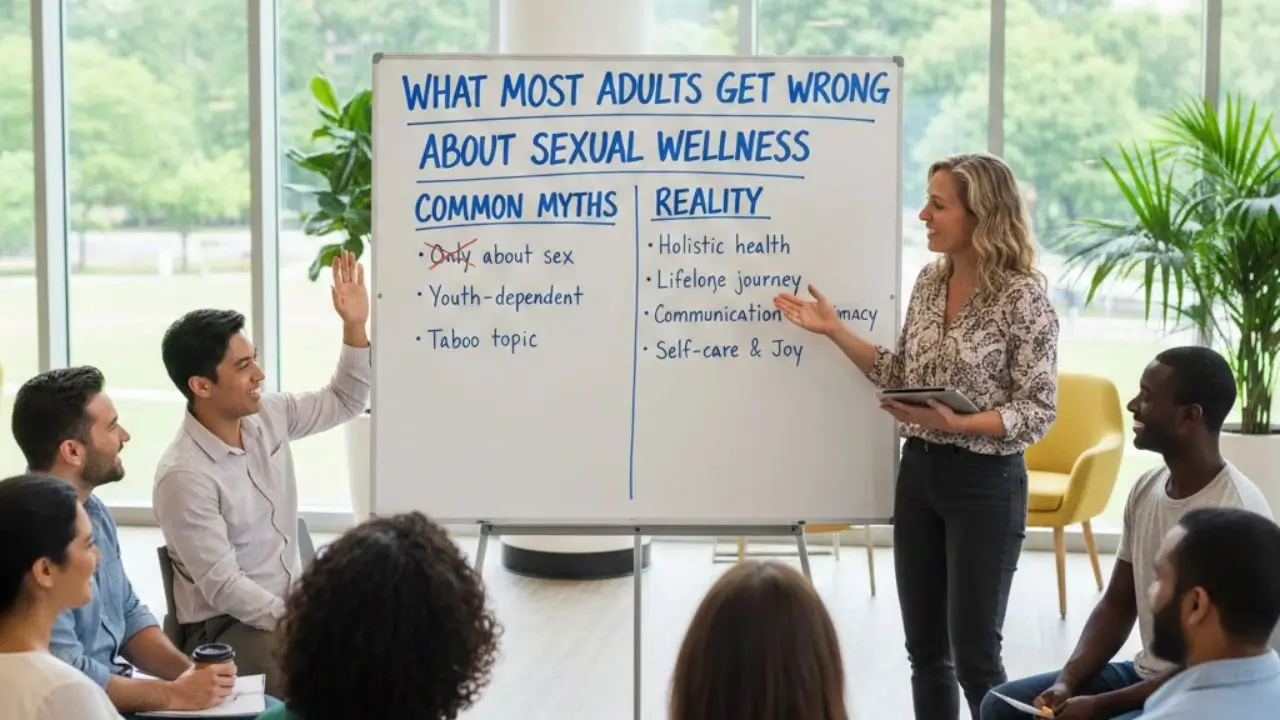
| Myth or misunderstanding | What doctors say is true | Why it matters |
|---|---|---|
| Sexual health is only physical | Emotional and psychological factors are equally important | Stress, anxiety, and relationship dynamics affect satisfaction |
| You can see if someone has an STI | Many infections show no symptoms | Testing is essential even when partners seem healthy |
| Condoms make sex completely risk-free | They greatly reduce risk but are not perfect | Correct use and additional precautions improve safety |
| Birth control prevents STIs | Hormonal methods prevent pregnancy, not infection | Barrier protection is still needed |
| Sexual problems are rare | They are common and often treatable | Seeking help can improve quality of life |
| Talking about sex is shameful | Open discussion leads to better outcomes | Communication supports consent and care |
| Performance equals worth | Sexual experiences vary widely | Reduces pressure and anxiety |
| Certain situations are “safe” from pregnancy or infection | Risk can still exist | Awareness prevents surprises |
Sexual Health Isn’t Just About Physical Function
Doctors frequently remind patients that desire, arousal, and satisfaction are influenced by far more than anatomy. Mental health, fatigue, medication, body image, cultural expectations, and unresolved conflict with a partner can all shape sexual experiences.
When people assume the issue must be purely physical, they may overlook treatable contributors such as depression or chronic stress. A holistic approach often leads to better solutions, whether that means therapy, lifestyle adjustments, medical treatment, or improved communication at home.
You Can’t Tell Someone’s STI Status By Appearance
One of the most persistent myths is that infections are always visible. In reality, many sexually transmitted infections remain silent for long periods. A person can feel completely fine and still pass an infection to someone else.
Because of this, doctors stress routine screening based on risk factors, not guesswork. Honest conversations with partners and regular checkups are far more reliable than assumptions based on how someone looks or feels.
Condoms Are Foolproof — Or The Only Protection You Need
Healthcare providers strongly support condom use because it significantly lowers the chances of both pregnancy and infection. But “significantly lower” does not mean zero. Breakage, slippage, or incorrect use can happen, and some infections spread through skin contact in areas not covered.
That is why professionals often recommend combining strategies: consistent condom use, vaccination when available, and regular testing. Layering protection provides a stronger safety net than relying on a single method.
Birth Control Does Not Protect Against STIs
This misunderstanding shows up often, especially among couples who use hormonal contraception. Pills, implants, and intrauterine devices are highly effective at preventing pregnancy, but they do nothing to stop infections.
Doctors encourage people to separate these goals in their minds. Pregnancy prevention and infection prevention are related but different tasks, and they may require different tools.
The Idea That Sexual Problems Are Rare Or Abnormal
Concerns about libido, erections, lubrication, pain, or orgasm are extremely common. Yet many adults feel isolated when they encounter them. Shame can keep people from mentioning difficulties, even during routine medical visits.
From a clinical perspective, these issues are part of normal human variation. They may be linked to aging, hormones, medications, or emotional strain. In many cases, they are manageable with proper guidance. Silence, however, can make them feel overwhelming.
Talking About Sexual Health Is Embarrassing Or Taboo
Avoiding conversation can create more harm than the problem itself. Doctors see how misunderstandings between partners lead to resentment, fear, or incorrect assumptions about attraction and commitment.
Clear, respectful communication helps couples express boundaries, preferences, and concerns. It also makes it easier to seek medical advice early, before small problems grow into larger ones.
Desire And Performance Are Not Measures Of Worth
Cultural narratives often tie identity to sexual ability. Men may feel pressure to maintain constant readiness; women may worry about matching unrealistic expectations. These beliefs can create cycles of anxiety that interfere with enjoyment.
Professionals emphasize that there is no universal standard for frequency or response. What matters is mutual consent, comfort, and satisfaction. Letting go of comparison can be liberating.
Other Everyday Myths People Still Believe
Doctors also encounter confusion about when pregnancy can occur, the risks associated with oral sex, and the reliability of withdrawal. While risk levels may differ, none of these situations are completely free of possibility.
Another lingering misconception is that masturbation is harmful. Medical experts generally consider it a normal behavior that can help individuals understand their bodies and reduce stress.
Building A Healthier View Of Sexual Wellness
Accurate information changes the way people approach intimacy. When adults understand that variation is normal and support is available, they are more likely to ask questions and advocate for themselves.
Routine checkups, vaccinations, and screenings form the medical foundation. Equally important are empathy, honesty, and patience between partners. Together, these elements create an environment where sexual well-being can improve rather than become a source of worry.
When To Seek Professional Advice
Doctors recommend reaching out whenever pain, sudden changes in desire, persistent performance concerns, or fear of infection arise. Waiting rarely makes issues disappear. Early guidance can prevent complications and offer peace of mind.
Healthcare providers are trained to handle these topics confidentially and without judgment. What may feel awkward to a patient is an everyday conversation in a clinic.
The Takeaway
Much of what adults believe about intimacy comes from rumor, media portrayals, or incomplete education. Medical professionals continue to repeat a simple message: sexual wellness is broader than mechanics, and myths can stand in the way of safety and satisfaction.
Replacing assumptions with evidence encourages smarter choices, healthier relationships, and greater confidence. A willingness to talk openly — with partners and with doctors — remains one of the most powerful tools anyone can use.






No Comments Yet
Be the first to share your thoughts.
Leave a Comment